If you have difficulties viewing this email, please view online |
August 2012 |
|
| |
 |
|
| |
 |
Graeme Osborne at a seminar in Auckland.
|
Trust is at the heart of the eHealth vision.
This issue of trust has been at the forefront of people’s minds during the seminars on electronic sharing of health information which we have held recently. Trust that health information will be made available securely without impacting the paramount relationship between consumers and their health professionals.
We knew from earlier seminars that people supported the concept of sharing information so the 2012 seminar series is an opportunity to provide updates on progress, further raise awareness of the benefits of sharing relevant health information, and gather feedback.
|
I have been heartened by people’s willingness to engage with these issues and we look forward to investigating them further as we work toward the Government's aim of all New Zealanders having access to their electronic health records by 2014. To read more about the seminars - and to view a short DVD about the benefits of electronic sharing of health information - visit www.health.govt.nz/sharedhealthinfo.
For a consumer perspective on themes emerging from the seminars, click here

The seminars have also been an opportunity to introduce our Connected Health brand to the public and sector. We currently use the brand for the exchange of secure information via telecommunications and have decided to expand its use to also cover the wider sharing of health information. There has been wide support for the term Connected Health. Wherever this brand is displayed, our goal is for people to have confidence that the health service or system is working to common standards to ensure the safe and secure sharing of health information within the wider health eco-system.
As I mentioned in the previous newsletter, work is underway on an updated National Health IT Plan outlining how the eHealth environment will look in 2014. The updated plan will be a refinement of the original. It will reflect the progress by the sector, and signal the critical deliverables for the future to achieve the eHealth vision.
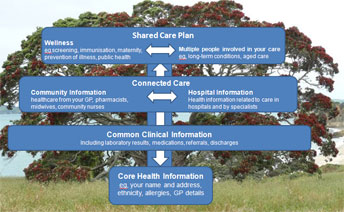
We have also developed a visual description of the eHealth IT solutions required to deliver the eHealth vision, in the form of a 'tree' with four levels which build on each other to provide a connected, effective eco-system. An individual's core health information provides the 'roots' for the tree, followed by common clinical results, connected care, and a shared care plan.
Graeme Osborne
Director
National Health IT Board
| |
|
|
| |
 It has been really valuable to hear clinical perspectives on electronic sharing of health information at the seminars we have held around New Zealand recently. It has been really valuable to hear clinical perspectives on electronic sharing of health information at the seminars we have held around New Zealand recently.
These perspectives have been provided at the public and community seminars, with members of the National Information Clinical Leadership Group (NICLG) appearing alongside members of our Consumer Panel to share their stories of clinical practice and talk about how electronic sharing might work.
We have also been able to engage with a wide range of clinicians at district health board briefings in several centres, including Taranaki, Waitemata and Counties Manukau. These have typically been attended by DHB staff, providers and vendors, and have provided an excellent forum to discuss issues directly relevant to the specialist audience.
We have also been seeking clinical input into the refresh of the National Health IT Plan which is underway, with discussion about clinical priorities taking place within NICLG and feeding into further work on the plan.
Finally, I was delighted to hear of the successful launch of the New Zealand Medicines Formulary in July by the Associate Minister of Health, Peter Dunne.
The formulary provides a one-stop shop of up-to-date information about subsidised and non-subsidised medicines used in New Zealand, and provides guidelines, protocols and other key decision support tools. It is a welcome resource for clinicians prescribing, dispensing and administering medicines.
In time, the formulary will be incorporated into clinical health IT systems, including prescribing and dispensing software, and this will further enhance its value to clinicians and consumers.
|
|
| |
|
|
| |
|
|
|
|
| |
|
|
| |
Highlights
|
|
| |
New Zealand Formulary launched
'GP2GP' achieves 2400 transfers in July
|
|
| |
|
|
| |
In this issue...
|
|
| |
|
|
| |
|
|
| |

HISO membership
HISO is pleased to announce the reappointment of Darren Douglass to the Committee. Darren has been granted a second term of 24 months on HISO from 25 August 2012. Darren represents the DHB Chief Information Officers Group.
In June, HISO approved the publication of the third part of the Health Information Security Framework Standard 10029.
Initially the standard was comprised of two parts, 10029.1 - Essentials and Recommendations and 10029.2 - Templates and Samples. The third part of this standard is the Technical Specifications Register.
This standard identifies requirements for implementing technical components of the Health Information Security Framework and is available on the HISO website.
HISO's support of clinical integration
Health information standards support the increasing need to safely and securely exchange a wide variety of patient information between various health care providers. Adopting a standardised approach to health information across the health and disability sector assists clinical integration and implementation of the National Health IT Plan.
Engagement with the Ministry and the sector is in full swing on a number of standards, either being reviewed or developed, that support clinical integration.
Due to an increasing awareness of the benefits of engaging with HISO, advice is being sought during the early stages of projects within the Ministry and the sector.
Details of these and the other current areas of HISO work can be found here. |
|
|
| |
|
|
| |
|
|
|
| |
| |
| Patients First update |
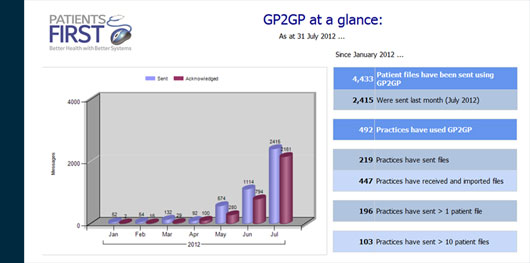
The GP2GP programme is experiencing rapid growth, with 492 practices now involved. GP2GP allows the transfer of a patient’s files electronically from one general practice system to another.
At a glance:
|
Clinicians and vendors seek IT solutions
The race is on to find workable information technology solutions to some of the problems health professionals face in their day-to-day practice.
Clinicians from around the country have identified work-related problems they believe would respond to innovative use of information technology, with 55 entering this year's Clinicians' Challenge.
The Challenge is run by Health Informatics New Zealand (HINZ), the New Zealand Health IT Cluster, and the NHITB.
Graeme Osborne, NHITB director, says the idea is to connect clinicians and vendors so they can produce creative, effective solutions to real-life problems.
"Having clinicians involved in the development of IT solutions to problems they face in the course of their work is more likely to guarantee the success of the systems that are developed," he says.
"The Challenge is also an opportunity for vendors to understand the problems clinicians face and come up with solutions that will make a real difference to health care in New Zealand."
The judges are Graeme Osborne, Peter Gow (National Information Clinical Leadership Group), Inga Hunter (HINZ), Dougal McKechnie (NZ Health IT Cluster), Denise Irvine (HINZ), and Angela Lim (consumer representative).
They will shortlist the entries received and send the best three to health IT vendors, who will have until 8 October to develop practical IT solutions. Vendors can submit their ideas through the HINZ website, www.hinz.org.nz.
The winning clinician and vendor will be announced at the HINZ conference in November. |
| |
|
| |
 Each year Counties Manukau DHB helps more than 8000 babies come into the world – and the DHB's head of maternity services says their mothers will benefit from moves underway to improve electronic sharing of health information.
Each year Counties Manukau DHB helps more than 8000 babies come into the world – and the DHB's head of maternity services says their mothers will benefit from moves underway to improve electronic sharing of health information.
Debra Fenton, the manager of Primary Maternity Services at the DHB, says the development of a new national Maternity Clinical Information System (MCIS) will improve the way clinicians manage the risks before, during and after childbirth.
"It will mean women having babies receive more efficient care because all their relevant health information will be at the fingertips of the health professionals involved in their care," she says.
Counties Manukau is keen to be one of the 'early adopters' of the new national system which is being developed by DHBs and the NHITB.
NHITB Director Graeme Osborne says the new system will help DHBs meet their clinical and reporting requirements, provide cost savings, and improve the quality and safety of their health services.
"There's a need for electronic information at the clinical work place to support safe, effective and efficient maternity practice for DHB-based maternity clinicians," he says.
Debra Fenton says her DHB reviewed its existing information system several years ago, quickly identifying barriers in the way it was collecting and documenting information.
"There were gaps in terms of the system's interoperability and not meeting the functionality of our work flow," she says. "We looked at the various options, which included trying to improve the existing system or developing a new one. At that point the National Health IT Board began looking at the possibility of a national maternity clinical information system, so the timing was perfect."
Debra Fenton says the DHB supports a wide range of clinicians across primary, secondary and tertiary services, and the current processes for sharing relevant health information are ineffective.
"Quite often women in pregnancy have to repeat information every time they see a different health professional because clinical documentation is not readily available. This is not ideal for the woman or the clinicians who are trying to plan her care to manage any risks she may have concerning her health or the health of her baby.
"The new system could potentially improve the standard of care significantly, and it's very exciting to be involved with this initiative." |
| |
| |
| Patient portal proves its worth for Wellington general practice |
A GP practice in Wellington is at the forefront of moves to share information electronically with patients. The Island Bay Medical Centre says its patient 'portal' proved so successful during a trial run the practice now wants to offer it to everyone on its books.
Dr Richard Medlicott says 170 patients have been using the portal, some of them since March 2009, and in a few weeks it will be available to all the practice's 4500 patients who have already consented to the medical centre's texting service.
Patients will be able to log in to the following link to read their diagnoses, list of medicines, laboratory results and comments, schedule of recalls, immunisations and medical alerts: ibmc.co.nz/ManageMyHealth
|
 |
Their GP's notes are not placed on the portal but Dr Medlicott says that’s because doctors use the notes to jog their memory and keep a summary of salient information when seeing patients, and it may not be a full reflection of all that is said in a 15-minute consultation.
Patients will be able to use the portal to make appointments with their GPs, order prescriptions, email their GP with questions about their health care, set health targets, and keep a journal and a calendar of health appointments and events.
 "It's a great tool for patients and it's helping the practice save time by doing electronically some of the things we'd normally do over the phone," says Dr Medlicott.
"Patients are able to send me a quick message if they want to check something or they can log on to see their lab results without having to wait for someone to ring them. Requesting prescriptions electronically frees up our nurses' time. Online appointment booking saves the receptionist’s time."
"It's a great tool for patients and it's helping the practice save time by doing electronically some of the things we'd normally do over the phone," says Dr Medlicott.
"Patients are able to send me a quick message if they want to check something or they can log on to see their lab results without having to wait for someone to ring them. Requesting prescriptions electronically frees up our nurses' time. Online appointment booking saves the receptionist’s time."
He says the portal enables patients and GPs to feel more connected, while being able to ask questions and respond in their own time. A major plus for patients is the absence of advertising on the portal and the lack of 'data mining'.
Dr Medlicott says he has agreements in place with some of his patients that they will pay attention to important information coming to them through the portal. For instance, he asks some of his patients on warfarin to open emails about their laboratory results, and they are asked to sign a consent form agreeing to do this.
His advice for other practices considering a patient portal?
"Develop a plan, start with a small group of patients first to get used to the process, and have good systems in place to make sure it runs smoothly, especially when doctors are away and cannot respond to queries," he says. |
| |
|
| |
 The new director of the country's national eMedicines programme believes technology can make a real difference to the quality and safety of health care.
Anton Venter, a registered pharmacist, is leading the national medication safety programme delivered jointly by the NHITB and the Health Quality & Safety Commission.
The new director of the country's national eMedicines programme believes technology can make a real difference to the quality and safety of health care.
Anton Venter, a registered pharmacist, is leading the national medication safety programme delivered jointly by the NHITB and the Health Quality & Safety Commission.
He's excited by the possibilities of his new role.
"It's very much about working with clinicians and DHBs to use technology to minimise patient harm," he says.
His priority is to support implementation of the 'Go for Gold' campaign. This aims to have all public hospitals participating in electronic medicines management and to have achieved 'gold' level medication management by the end of 2014.
Gold level is when a hospital has implemented medicine reconciliation (eMR) and electronic prescribing and administration (ePA). The widespread use of eMR and ePA will reduce the number of New Zealanders harmed each year by medication errors and adverse drug events.
"I'll be focusing on understanding what support DHBs and clinicians need to take part in the 'Go for Gold' campaign and what obstacles need addressing," says Mr Venter.
A DHB readiness assessment underway will provide information and insights into what DHBs already do well and where they need assistance.
"DHBs have a lot of competing priorities and often have to make hard decisions, so the next step involves working really closely with them to see what practical help we can offer."
Anton Venter says his new role is a logical extension of his work as a hospital pharmacist, his postgraduate studies in clinical pharmacy at Otago University, and the work he has done in change management and the implementation of IT-enabled health services.
"It's all about making a positive difference to the way people experience health care," he says. |
| |
| |
|
Information Governance EAG to provide input
The Information Governance Expert Advisory Group (EAG) has started its work in developing a framework for the safe sharing of health information, with an initial round of meetings to familiarise itself with the pressing issues.
The EAG was established to develop policy and guidelines for a health information governance framework, and to provide some clear guidance to the sector on how health information should be shared. Recommendations will be made to the NHITB.
EAG members include the Chair, Barbara Phillips (Ministry of Health), Sandra Hicks (NZ Medical Association), Denise Irvine (Nursing Council), Lyndy Matthews (Council of Medical Colleges), Ernie Newman (Consumer Forum), Sebastian Morgan-Lynch (Office of the Privacy Commissioner), Inga Hunter (General Practice NZ and Royal NZ College of GPs), and Sharron Cole (Midwifery Council). A representative from the DHBs has yet to be appointed.
Tony Cooke, Manager Health Systems Investment and Planning, e-Health Programme, says the need for an EAG was identified more than a year ago.
"The need for a clear understanding of how health information can be shared safely and securely is key to the success of the National Health IT Plan," he says. "We're expecting lively, informed discussion of key issues facing consumers, clinicians and health leaders in the health information environment, and this group will provide us with valuable insight into the decisions we need to make." |
| |
|
| |
 Forum for IT vendors
Forum for IT vendors
Health IT vendors took part in a forum organised by the Health Identity Programme at the end of July.
A total of 35 people from around New Zealand participated via video conference, and Wayne Woodfield, Group Manager Health Identity, says the forum was a success.
"It's a great way for us to talk directly to people in the sector and involve them in our work without tying up people’s time or limiting attendance based on the physical location of the forum," he says.
The forum provided updates on key areas of health identity activity, including the programme's progress, timeframes, SSR gateway remediation, business-to-business gateways, and how changes in search behaviour affects customers.
Guest speaker, GP Dr Ashwin Patel, discussed his experience of integrating the new Health-e-Address web services into six of his GP customer sites as part of the Health Identity Programme's early adopter trial.
"The technical side of integrating the Health-e-Address web services was very straightforward," Dr Patel told vendors at the forum. "I don't expect patient management system (PMS) vendors will have any difficulty integrating it.
"The information in it is better than what they have currently. It deals with rural addresses and post office boxes-, more accurately, with information from referenced databases."
District Health Boards can obtain the Health-e-Address specifications by emailing identity@moh.govt.nz.
Requirements for new web services – patient and provider indexes
The Health Identity Programme has drafted requirements for the web services that will enable interoperability between health sector systems and the Patient and Provider Person Indexes. These requirements documents form the basis for a Web Service Definition Language (WSDL). Feedback on the documents close on 17 August.
The information will be updated and reissued as final documents with a corresponding WSDL. After this, the Health Identity Programme will look for a group of early adopters who are interested in accessing the indexes via this service. To express your interest, please email identity@moh.govt.nz.
Health Provider Index
The new Health Provider Index system, developed by the Health Identity Programme, replaces the Health Practitioner Index. It is called the Health Provider Index (HPI) as it has the future capability to extend beyond registered practitioners to include other people working in the health and disability sector.
The health system relies on this HPI database for information about registered health practitioners and the organisations that employ them. Practitioner data is currently provided by Responsible Authorities, such as the Medical Council or Dental Council. The database is mostly used by DHBs and agencies such as the Accident Compensation Corporation (ACC), large laboratories and the Institute of Environmental Science and Research (ESR).
The new system will also enable many DHBs, hospitals and community laboratories to have online access to the HPI for the first time.
Currently data is received and returned via a manual process, administered by the Ministry of Health. With the new system, the transfer of this information occurs through web services.
It is important to note the Common Person Number (CPN) that is assigned to each practitioner remains the same.
More information about the Health Provider Index is available here. |
| |
| |
|
Emerging themes from shared health information seminars
The NHITB has nearly completed a series of public and community seminars to discuss improvements to the way personal health information is shared electronically.
Ernie Newman, Chair of the NHITB's Consumer Panel, says people using health and disability services will benefit greatly from these improvements.
"It means that clinicians caring for us will, with our consent, have access to all of our core health information over the course of our personal health journey," he says.
"We will also be able to access our own records and take a greater role in managing our own health and wellness."
There was widespread support for the concept of electronic sharing of health information. Ernie Newman says issues which will need to be resolved to ensure public confidence include:
- questions about security and confidentiality, and who will have access to the information
- the possibility of some information being 'sealed' to protect privacy and further restrict who can view it
- questions about how long data will be stored
- concern about other services gaining access to personal information
- issues raised by particular community groups – eg Pacifica peoples seeking assurances about citizenship databases and Asian families concerned about access to an elder's health status within the family.

Ernie Newman |
| |
|
|
|
|
|
| |
|
 |
|
